Grateful thanks are given for the historical records of Drs. William H. Spencer, and Jerome Bettman, along with important contributions from Drs. Alan Scott, and Robert Stamper

In 1855, toward the end of California’s Gold Rush, Dr. Elias Samuel Cooper inaugurated Cooper’s Eye, Ear and Orthopaedic Infirmary in San Francisco, going on to found the first medical school in the far west in 1858, which was named The Medical Department of the University of the Pacific. In 1870 Dr. Levi Cooper Lane who had joined the school’s faculty in 1861, was appointed acting professor of ophthalmology and otolaryngology.
“No local anesthetics were available. It would be 11 years before Kohler learned the value of topical cocaine from Sigmund Freud. Both ether and chloroform had been in use. There was no known medical therapy for glaucoma. Cataract operations had been described by Jacques Daviel over 200 years before, but much of the operation was conditioned by the absence of anesthesia, thus the essence was speed.”
Jerome Bettman, MD, “Vis a Tergo” speech

The ophthalmology department was started in 1872 when Adolph Barkan was appointed as the first professor of ophthalmology and otolaryngology. He would later continue in the same position at Cooper Medical College and at Stanford University Medical School. Over a hundred years later the residency’s alumnae association would be named The Barkan Society in his honor.
The Cooper Medical College eventually spawned the eye departments of both Stanford, and the University of California in San Francisco. Dr. Lane funded a new medical school building at Sacramento and Webster streets in San Francisco in 1882, however, by the time of his death in 1902, the lack of financial resources caused the school to search for a university affiliation. This was the first of many financial crises which would affect the development of the training program. In 1908 Stanford University accepted Cooper Medical College as its Department of Medicine although complete control did not pass from the directors of Cooper Medical College to the trustees of Stanford University until 1912.
Dr. Adolph Barkan retired in 1912 and returned to Vienna and Dr. Albert B. McKee was appointed by Stanford University as his successor. Meanwhile, Adolph’s son Dr. Hans Barkan returned from training in Vienna and joined the eye department faculty in 1915, going on to succeed McKee as Department Chair in 1928. Notably, another son, Dr. Otto Barkan was also an ophthalmologist who was known for his surgical innovations. Hans Barkan is credited with establishing a formal ophthalmology training program in 1917. His tenure was marked by the early presence of woman residents.
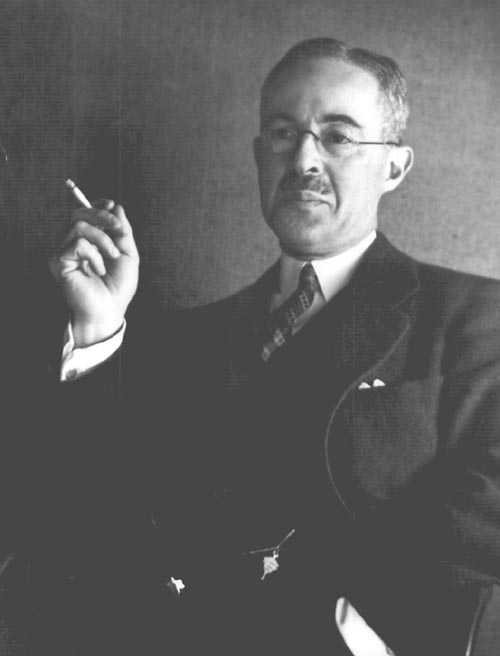
When the hugely influential Dr. Alfred E. Maumenee succeeded Hans Barkan as eye department chair in 1948 he brought with him sweeping changes in teaching styles, rejecting autocratic Viennese methods. During his 7-year tenure he emphasized research and clinical work ultimately finding himself in conflict with Stanford’s vision of ophthalmology. Maumenee left California to become Chairman of the Wilmer Institute at Johns Hopkins in 1955 where he served until 1979.
 “When I went to California, I found that most of the senior ophthalmologists had been trained in Vienna where you could never argue with the professor…I brought out the idea that you’re supposed to argue. I had rounds on Monday mornings, and many practitioners in town came to them. We would argue with the faculty and fight back and forth…”
“When I went to California, I found that most of the senior ophthalmologists had been trained in Vienna where you could never argue with the professor…I brought out the idea that you’re supposed to argue. I had rounds on Monday mornings, and many practitioners in town came to them. We would argue with the faculty and fight back and forth…”
Alfred E. Maumenee, MD, Oral History
Dr. Dohrmann K. Pischel, an excellent teacher and leader in the field of retinal detachment who had mentored Maumenee, succeeded him as departmental chair from 1955 to 1958. These were turbulent times as Stanford Medical School was making plans to move from San Francisco to their new campus in Palo Alto.
The medical school’s move coincided with the initiation of a new national trend toward staffing American medical schools with employed full and/or part-time physicians. Consequently, relatively few members of the San Francisco based medical community moved to Palo Alto while the ophthalmology training program continued in Palo Alto as a division of the Stanford department of surgery.

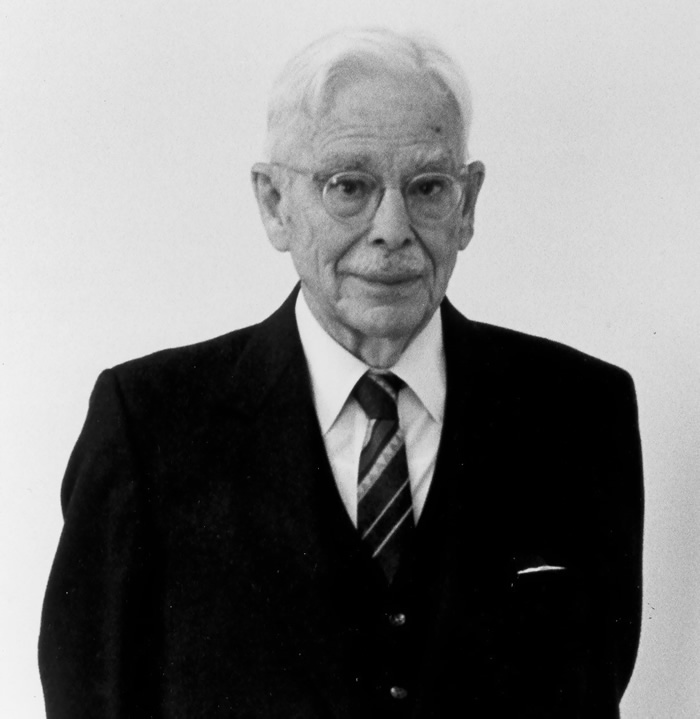
Dr. Jerome Bettman succeeded Dohrmann Pischel in 1958 and soon had a full-blown crisis on his hands. Stanford had moved their medical school, leaving behind empty facilities, an eye clinic stripped of equipment and a faculty in some disarray.
“The days of Stanford in San Francisco were coming to an end and the medical school moved to Palo Alto in 1959. The burden of preserving a Department of Ophthalmology on Clay Street fell to me. 76% of the Stanford faculty elected to remain in San Francisco. Stanford was willing to permit us to use and eventually possess the structures that comprised their San Francisco School, but they were to take all equipment, and made the stipulation that we in San Francisco could not solicit funds.
Several of us met at the home of Henry Gibbons III, the grandson of the first professor of medicine. If Stanford could be persuaded to retain their half of the San Francisco General
Hospital and the Veterans Hospital for our use, we would have plenty of material to enable us to carry on with a teaching institution. For reasons of their own, Stanford would not.”
“I shall not forget that dismal night of the second meeting at the home of Henry Gibbons. It was one of those bone-chilling foggy nights in San Francisco. We had lost the San Francisco General and the Veterans Hospitals; Stanford was to remove all equipment;
the Clinic was always a money-losing venture, but now, we were not permitted to solicit funds. We had fallen upon evil days!”
Jerome Bettman, MD, “Vis a Tergo” speech

Within a year, all of Stanford’s San Francisco facilities were transferred to a non-profit corporation sponsored by the Presbytery of San Francisco, renamed Presbyterian Medical Center (PMC). Bettman went on to solicit donations for equipment, form affiliations with Alameda County’s Highland Hospital, which continues to today, along with the Southern Pacific Hospital, Children’s, and Mt. Zion’s hospitals. He was also able to institute a basic science teaching program assisted by Dr. Michael Hogan, chairman of the University of California Medical School. Bettman nurtured the excellent faculty which had long participated voluntarily in clinical activities on a part-time basis, including Drs. Max Fine, Ernest Denicke, Dohrmann Pischel, Thomas Ferguson and the pioneering researcher Dr. Arthur Jampolsky who had been a resident at Stanford under Maumanee. Jampolsky shared clinical space with Barkan and Bettman and strabismus cases and research ideas with Dr. Edward Tamler who had also worked with Maumanee.
“What were the Ophthalmology residents to do as 1960 rolled around? We met and agreed that there was every reason to continue the program that existed if possible…the hospital was able to fund the resident salaries. – the senior resident got $280/month, so we didn’t cost much! It was an exciting and interesting transition time, to which many persons contributed significantly, making the community-based department which continues today.”
A resident’s memory – Dr. Alan Scott

Integral to the phoenix-like rising of the department of ophthalmology was the Lions Eye Foundation for Children, Inc. The Lions stepped in to fill the financial needs of the clinic which was devoted to the care of underserved children and soon, adults as well. Later the foundation was re-named the Lions Eye Foundation of California/Nevada, Inc.http://www.lionseyeca-nv.org/ which continues today, providing significant funding for the Lions Eye Clinic now located at the PVF Eye Institute.

Between 1958 and 1966 the new medical center sought new affiliations and financial aid to build a new Presbyterian Hospital. The University of the Pacific had funded a dental school and planned a graduate school of medical sciences on the campus. Dr. Arthur Jampolsky succeeded Barkan as departmental chair in 1966, also directing the newly formed Smith-Kettlewell Institute of Visual Sciences since renamed as Smith-Kettlewell Eye Research Institute. Dr. Jampolsky was instrumental in recruiting Dr. Bruce Spivey as the next departmental chair.

In 1971, Dr. Bruce Spivey from the University of Iowa Medical School was named Chairman of the Department and Dean of the School of Medical Sciences at the University of the Pacific. A Vietnam veteran, he had served as a triage officer in a battlefield hospital, leading to his lasting commitment to international service. He had also achieved a master’s degree in Medical Education from the University of Illinois and had secured an NIH grant to explore the concept of a full-fledged medical school. The medical school was to have a unique competency-based education system which was quite a departure from the norm at the time. A basic science faculty was already present at the nearby University of the Pacific Dental School and the researchers at the then named Pacific Medical Center. Sadly, despite the radical but sensible idea of a competency-based education, the project had to be abandoned as medical school education became too expensive for the resources available.
The ophthalmology department however, along with medicine, psychiatry, surgery, and pathology, continued their roles as medical educators through residency programs, fellowships and externships for medical students from other institutions. For ophthalmology, there was to be a core full-time clinical faculty while most of the clinical teaching would continue to be done by the many, highly qualified community ophthalmologists who had been supporting the residency program in ophthalmology since its inception.
In 1972, the eye clinic was in the process of moving from the old Cooper-Lane Building (ca. 1880) to the Eye Department’s new home for the next 40 plus years on the fifth floor of 2340 Clay Street. The residency consisted of two residents each year admitted in staggered fashion. The residency was popular because of the excellence in clinical teaching and the friendly environment. However, few formal didactics were available within the department except for occasional Grand Rounds speakers. For didactic education, second year residents attended the Stanford basic science course held each summer in Palo Alto. This course was organized and led by Dr. Jerome Bettman and taught by academically inclined community ophthalmologists from around the Bay Area and the United States.

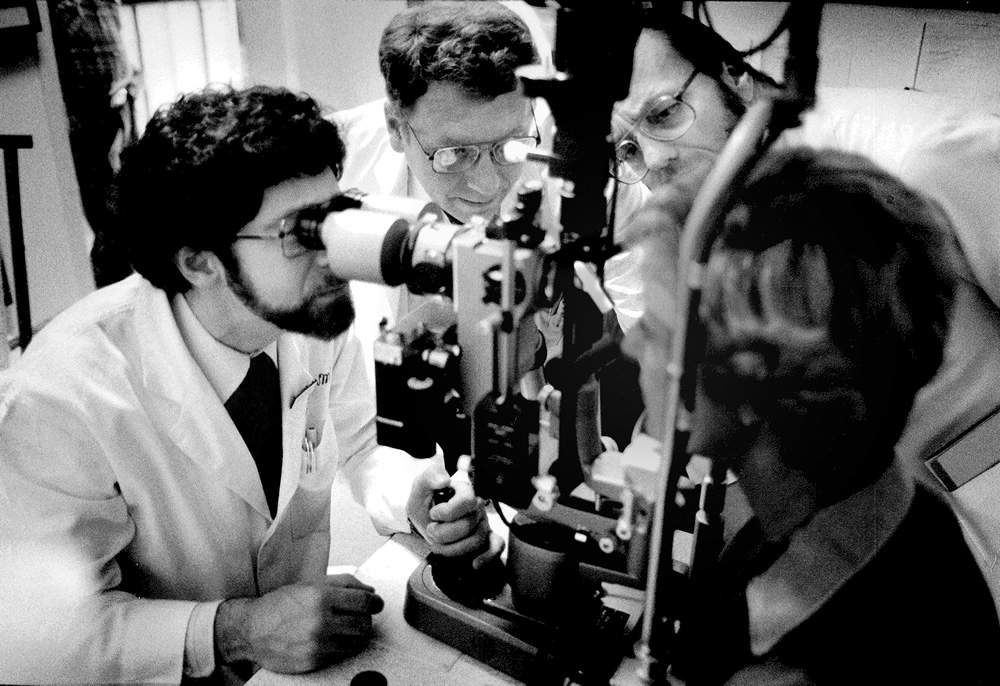
The clinical training in sub-specialties for the residency was directed over the next several years by a small cadre of full-time faculty which gradually grew. Led by Spivey, the group included Drs. Robert Stamper in glaucoma, Gus Colenbrander in low vision, Nancy M. Newman in neuro-ophthalmology, John Cavender in ophthalmic pathology and medical retina, William Spencer in pathology, along with Bob Webster, Rich Abbott, and David Vastine in cornea. Both Alan Scott and Arthur Jampolsky had been prominent researchers since the 60’s. This group formed the nucleus of a highly respected department with an international reputation, augmented in the next few years by the addition of William Stewart in ophthalmic plastic and reconstructive surgery, Everett Ai in retina and Susan Day in pediatric ophthalmology.
The 70’s and 80’s were taken up with organizing a formal curriculum for the residency, an in-house didactic program and strengthening the clinical teaching. Unlike many academic institutions, the full-time faculty and the volunteer faculty had a close, collegial, and congenial relationship filled with mutual respect and camaraderie. This atmosphere made a most enjoyable milieu for both faculty and residents which remains a hallmark of the residency. It must be noted however that a significant change in the practice of ophthalmology was happening during this time. The need for hospitalizations for ophthalmic surgeries was greatly reduced which in turn, reduced hospital revenues from eye patients and a lessening of ophthalmology’s influence in hospital management decisions. In 1972 twenty-five percent of hospital patients were occupied by ophthalmology patients.
In 1976, Presbyterian Hospital found itself in financial distress for a variety of reasons. and Spivey’s career path turned more complex as he was appointed President and CEO of the entire facility, in addition to his role as Chair of Ophthalmology. In 1977, Spivey’s strong administrative skills led to his appointment as the founding CEO/EVP of the American Academy of Ophthalmology and in the mid-nineties he led the revitalization of the International Council of Ophthalmology, serving as both Secretary General and then President. He was also named CEO of the California Healthcare System. Spivey went on to posts at Northwestern University Medical School and a combined position at Columbia and Cornell Medical Schools in New York City. In 1994 he received the Howe Medal of the American Ophthalmological Society (AOS) and 2015 he received the American Academy of Ophthalmology Laureate Award.

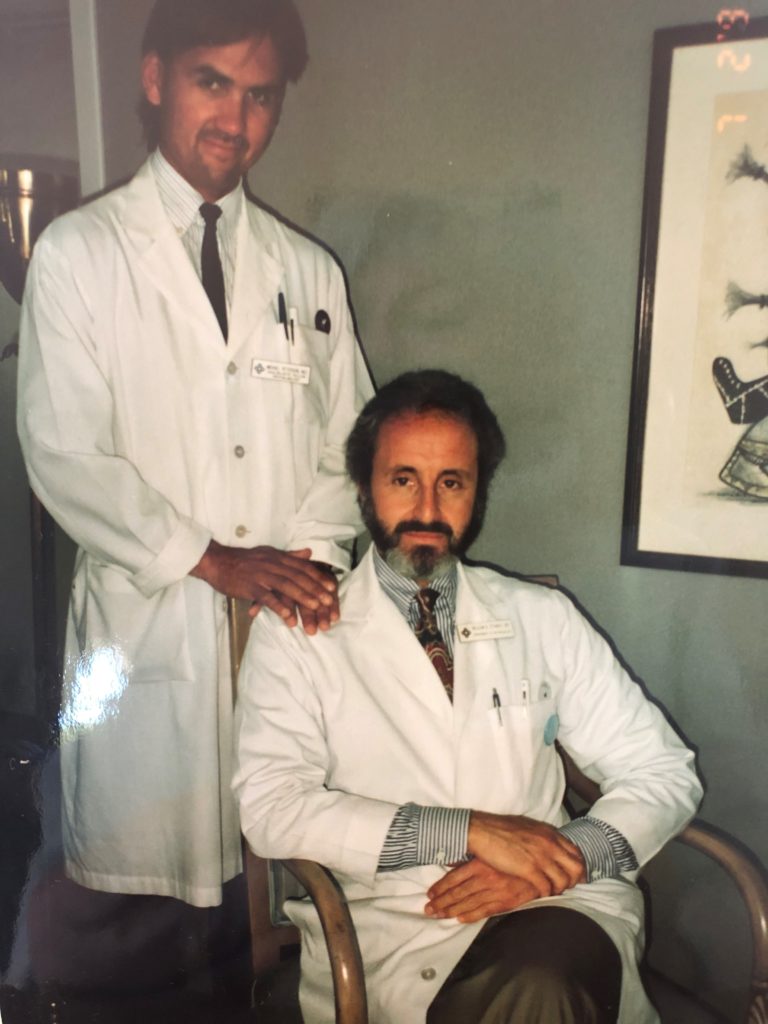
Dr. Robert Stamper was appointed as Director of the Residency program in 1972 and had succeeded Spivey as Department Chair in 1987. A graduate of SUNY, Stamper completed his residency and fellowship training in Glaucoma at Washington University St. Louis. He also served as Chief of Glaucoma from 1972 to 1989.
Stamper strengthened the faculty, focused on raising endowment funds for Pacific Vision Foundation and began the process of renovating the clinic’s facility at 2340 Clay Street. Stamper was also successful in convincing the Association of University Professors of Ophthalmology (AUPO) to grant full voting rights to the residency program, previously denied due to the program’s lack of affiliation with a medical school.
An important aspect of the training program was the experience provided by Highland Hospital in Oakland, first under the direction of Homer Brugge, who was succeeded by David Vastine and, for over 20 years, Richard Imes, followed most recently by alumnus Jonathan Hernandez. As a typical inner-city hospital, Highland provided a needed service otherwise unavailable to the medically indigent patients of Oakland. As an important Northern California trauma center, Highland Hospital provides an excellent opportunity for the residents to care for injuries and acute eye problems.
The Lions’ Eye Foundation continued to be central to the residency program as they paid for patients from all over Northern California and Nevada to come to the eye clinic for medical and surgical care that they otherwise could not afford or was not available in their area. The medical and surgical care of these patients was accomplished under the supervision of both the full and volunteer faculties and provided both a service to their community and learning opportunities for the residents which continues as a hallmark of the residency.
During Stamper’s tenure the hospital underwent a difficult retrenchment and the hospital abruptly cut back financial support for the ophthalmology residency program. Beginning in 1995 the full-time faculty was dismantled, coincident with the merger of the medical center with Sutter Health. Some of the full-time faculty found a welcome in the private practice of Pacific Eye Associates on campus and continued their clinical, research and teaching activities there. However, most ultimately moved on to positions elsewhere.
Stamper accepted a post as professor at UCSF where he is the Fortisure Endowed Professor. In 2007 he received the AAO Life Achievement Honor Award and in 2019, the Visionary Award from the Glaucoma Research Foundation.
Dr. William Stewart succeeded Stamper in 1996. He had graduated from the University of Minnesota and was an alumnus of the residency and completed fellowships in orbital surgery at Moorfield’s Eye Hospital and Bascom Palmer. Stewart completed the renovation of the Lions Eye Clinic and faced the challenges of transitioning to a new form of academically oriented eye care and looked to rediscover the culture of superior health care, volunteerism, philanthropy along with a commitment to education, clinical research, and community service.
Stewart was instrumental in creating the Ophthalmology Leadership Committee and the Core Faculty Group as governing bodies for the Department and successfully managed a financial re-organization. Working closely with the Lions Eye Foundation, he described the relationship between the Department, Lions and Pacific Vision Foundation as so intimate and intertwined that the Department’s well-being is inseparable from each organization.
In 1990 Stewart became the Founding Medical Director, for the Institute for Health & Healing, California Pacific Medical Center/SutterHealth Systemhttps://www.sutterhealth.org/services/holistic-integrative-medicine/institute-health-healing which today is recognized for its vital role in Sutter Health’s medical programs. Since 1983 he has served as a volunteer at the Aravind Eye Care System, Tamal Nadu, India which honored him in 2019 with the Dr. G. Venkataswamy Endowment Oration Award.

Dr. Susan Day was named Chair of the department in 2000. She had received her medical degree from Louisiana State University and is a 1979 alumna of the residency program. Day spent her fellowship with Mr. David Taylor, a consultant at Great Ormond Street Hospital, London and additional strabismus education with Dr. William Scott and Dr. Marshall Parks prior to returning to San Francisco.
Prior to being named Chair, Dr. Day had also served as Program Director, a dual responsibility she held throughout her tenure. Day infused the department with passion and energy, working to keep the voluntary faculty involved and committed to provide a unique, community-based clinical training program. Residents gain experience during rotations served at the Lions Eye Clinic, Highland Hospital in Alameda, San Francisco’s Kaiser Hospital, and through individual mentoring in the private practices of faculty sub-specialists.
Active in national activities, Dr. Day served as the first woman President of the American Academy of Ophthalmology as well as serving as President of the American Ophthalmological Society and the Association of University Professors of Ophthalmology and Board Chair of the Accreditation Council for Graduate Medical Education. She also provided critical support during the foundation of The Pacific Vision Eye Institute. Dr. Day currently serves as President, and CEO for ACGME International. She was awarded the Howe Medal by the AOS in 2016 and 2018 she was awarded the Marshall Parks Medal.

Having served as Interim Chair for a year following the departure of Dr. Susan Day, Dr. Kevin Denny, a graduate of Harvard College and the New York University School of Medicine, and an alumnus of the department, became Chair in 2015. He had served as Chief of Cataract Surgery for 15 years. Denny’s first five years as Chair were devoted to sustaining the department, while serving as an important liaison between faculty and the leaders of the Lions, CPMC and Pacific Vision Foundation in the quest to establish a permanent home for the residency and the Lions Eye Clinic.
Economic realities and construction challenges were continual as the PVF team led by CEO Ellen Jamason worked with The Robert Wood Johnson Foundation which had committed to a $10 million loan to help improve eyecare for the underserved in the San Francisco Bay Area and Northern California.
Denny’s leadership was instrumental as the Pacific Vision Eye Institute became a reality in 2016 when independent ophthalmology practices began relocating into offices at 711 Van Ness Avenue, followed soon after by the Education Center for Grand Rounds and seminars. The Lions Eye Clinic and Ophthalmic Diagnostic Services moved from their previous locations at California Pacific Medical Center into facilities for which the Lions Foundation generously donated new examination equipment.
The next major effort undertaken during Denny’s first term involved planning, funding, and building out the Pacific Vision Surgery Center intended to provide patients, residents, and faculty a dedicated and convenient eye surgical environment just steps away from the Lions Clinic. Denny credits Ellen Jamason and the PVF Board with getting the ASC up and functioning in the fall of 2020 despite the many challenges presented by the COVID pandemic.