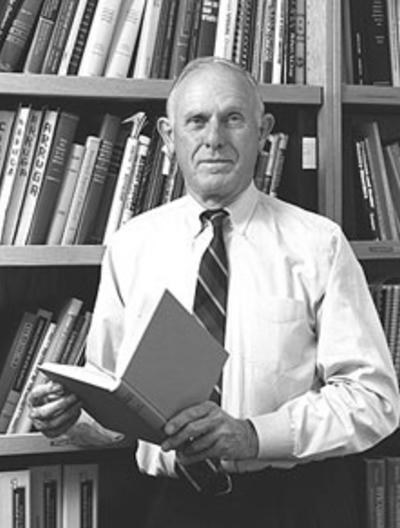
Alan Scott, MD
The story of Botox in his own words

In the 1960’s, the outcome of strabismus surgery was far from perfect, since as many as 40% of patients needed re-operation. No one knew the strength of a muscle, how much it contributed to the eye movement, what the nerve control signal provided, what parts of the muscle contracted, and so on.
With a brilliant engineer, Carter Collins, III, PhD, and a team assembled to construct mechanical and electrical apparatus, we set out to make these measurements on humans and to construct a rational model to guide strabismus surgery at Smith-Kettlewell, the eye research lab at CPMC.
One experiment was to inject anesthetic and see what happened to alignment and movements with paralysis of individual muscles. We developed Teflon coated injection needles which recorded the EMG from the tip, allowing us to find and inject specific muscles. These needles are used everywhere today to inject muscles accurately. After we became experienced with this, we began investigating different substances that could be injected into eye muscles of animals to weaken them, and then perhaps create permanent alignment changes.
Daniel Drachman, MD who is today the WW Smith Charitable Trust Professor of Neuroimmunology at Johns Hopkins, used botulinum toxin to study hind limb development in chicks. He injected small amounts into one limb without damaging the embryo elsewhere, which was just what we needed. Drachman had obtained toxin from Ed Schantz, MD who had brought his expertise on extracting toxins from the Army Chemical Corps to the University of Wisconsin where he was a professor of Food Microbiology and Toxicology.
Schantz generously supplied us with toxin for most of our subsequent experiments, clinical protocols, and early lots of Botox®. Clinical botulism epidemics showed that, of the 7 botulinum toxins, type A toxin created the greatest muscle paralysis, so we chose type A to work with. After we defined potency and effect on mice, and cats, I injected muscle and altered alignment became apparent. The muscle weakness was restricted to the target muscle and lasted several weeks. The exciting outcome was altered eye alignment lasting months! There were only a few local side effects and no apparent systemic toxicity.
We could immediately see the value of botulinum toxin in strabismus and realized that it would be useful in blepharospasm and many other conditions of muscle overactivity. We reported these results in a 1973 paper. We conducted subsequent studies to assess the stability, dosing, and toxicity of the toxin, in order to formulate it as a drug for human use. We changed the protein stabilizing agent from gelatin, an unapproved animal product, to human serum albumin.
Although the toxin amounts were initially given in nanograms or micrograms, we moved fairly quickly to using units based on the mouse LD (50) test because we were interested in the biological activity. We had a good idea from our animal usage of the doses to use in patients and went on to develop a freeze-dried product that was safe in amount and stable over time. Our IND (Investigative New Drug) Application lay on some FDA desk for almost 4 years! David Cogan, MD, had moved from Harvard Chair of Ophthalmology the NIH as a senior scientist and investigator. He kindly put in a word supporting our application and it was approved in a few days.
Despite extensive experience characterizing toxin and injecting many animals, it was still an experience to inject the first human patient in 1978. He had undergone retinal detachment surgery and was left with an eye pulled to one side. The CPMC protocol required us to keep him in the ICU for 3 days after the injections. The initial small dose straightened the eye, lasted a few weeks, and created no complications. So, one patient in 1978, 12 in 1979 and then the gates opened, and patients came in abundance.
After success in strabismus, I did the initial injections for blepharospasm, hemifacial spasm, torticollis, and limb injections for multiple sclerosis patients with spasticity in the hip muscles. Soon, 20 ophthalmologists at a time came to free seminars where we taught EMG injection technique. Physicians beyond ophthalmology became interested in using toxin for neurological, urological, GI conditions, cerebral palsy, excess sweating and more. We wound up running an open trial with over 200 investigators using over 10,000 vials annually.
It became obvious that we needed to increase our manufacturing capability, even though my primary interest was in research and not in developing a product. Our lab had a patent policy under which we declared items or processes of possible patentability. However, the lawyers told us that our 1973 paper had disclosed how toxin worked, thus precluding a later patent, even though that 1973 paper was published years before demonstration of clinical effectiveness, so we never got a patent.
Without a patent, no pharma company would take over manufacturing. So, I took out a loan on my home and developed a corporation, Oculinum Inc., to handle this project. Good fortune brought Dennis Honeychurch to oversee product development in 1983. Dennis had experience with GMP (Good Manufacturing Practices) in his work as a radio-pharmacist with the Navy. We needed a product license and an establishment license issued by the Food and Drug Administration (FDA) Center for Biologics, typically issued to large corporations. The project was moved out of the research facility and into a more suitable location in Berkeley across the street from an animal testing facility.

The first step toward licensing was to create a manual to cover GMP and Quality Assurance, in total, more than 100 procedures. FDA allowed us to contract out some of the manufacturing steps to a facility in Albuquerque New Mexico as long as one of our staff was present during the process. Dennis or I would gown up and enter the clean room used for compounding. We were both immunized against the effects of the toxin and as such would make the first two critical dilutions. This provided a diluted toxin solution that was safe for the technicians to handle. While we went skiing at Taos, the technicians produced batches of 10,000 vials which were packaged with dry ice and shipped by air back to San Francisco. We were required to declare the dry ice as a hazardous item, but the botulinum toxin was exempt!
In the early days, we asked for donations of $25 for each vial of botulinum toxin type A that we sent out to other investigators and the money went to Smith-Kettlewell to pay for our research studies. After we hired additional personnel to help with the testing of multiple batches, the batch and clinical data and statistics on hundreds of cases, we raised the requested donation to $40 per vial. In 1987 we had to stop production as neither the Board at Smith-Kettlewell nor the insurers wanted the risk of us distributing toxin for humans.
By that time, hundreds of patients with blepharospasm, torticollis, spasmodic dysphonia and so on, were clinically dependent upon toxin. They were extremely upset and sent the FDA an avalanche of letters, which caused the FDA to wake up and get actively involved. We were off their radar and had not been visited for 5 years! Oculinum ™ (botulinum toxin type A) was licensed by the FDA on December 29, 1989 for the treatment of strabismus and blepharospasm associated with dystonia in patients 12 years of age and older. A pediatric ophthalmology consultant to FDA recommended that they disallow usage for children, even though we had supporting data on over 800 pediatric cases. It was a mistake on my part to let this pass, as childhood strabismus treatment with Botox® soon became widespread, but only outside the USA.
Allergan had a distribution agreement with Oculinum, Ind., from which it acquired the Oculinum® product in 1991. It was renamed Botox® in 1992. As predicted, Botox® has become a major pharmaceutical drug that has proved useful for dozens of conditions in which blocking abnormal nerve conduction is effective. About 55% of Botox® goes to these medical conditions, 45% to cosmetic use.
We went on to develop the non-profit Strabismus Research Foundation to continue work in San Francisco on alternative strabismus treatments. Injection of eye muscles with the local anesthetic bupivacaine to treat strabismus is the first major outcome from SRF. Two hundred forty clinical cases have shown bupivacaine to be more powerful than Botox® alone, with the combination of both drugs, one in the agonist, the other in the antagonist muscle correcting large deviations and creating alignment corrections lasting years with results fully comparable to surgical corrections.
